The Insights Report: January 14, 2026
 Insights on postsecondary institutions, Canada’s current and future workforce, and industry sectors.
Insights on postsecondary institutions, Canada’s current and future workforce, and industry sectors.
POSTSECONDARY INSTITUTIONS
Canadian colleges record their largest total revenue and spending increases in more than two decades
Canadian colleges recorded their largest increases in total revenue (+11.5 percent) and expenditure (+12.3%) in more than two decades in 2023/2024, according to a report by Statistics Canada (StatsCan).
Total revenues reached $18.5 billion, while expenditures totalled $17.9 billion.
Nearly four-fifths (77 percent) of the annual increase in college revenues came from student fees ($1.5 billion), followed by investment income (9.7 percent), provincial funding (seven percent) and other revenue sources (6.3 percent).
A $2-billion increase in college expenditures was largely driven by higher salaries and benefits (45.5 percent), followed by spending on fees and contracted services (31.4 percent), operational supplies (5.1 percent), and expenditure items (18 percent) such as utilities and furniture and equipment.
A record increase of nearly 100,000 new students contributed to the 23.2-percent increase in total college fees collected in 2023/2024.
Most of this growth came from international students studying in Ontario, who often pay up to four times more in fees than Canadian students.
Over the last two decades – particularly since the COVID-19 pandemic – colleges have become increasingly reliant on student fees as opposed to public funding.
In 2020/2021, fees accounted for less than one-third (32.9 percent) of total revenues; by 2023/2024, this share had risen to 42.1 percent.
Some variations in dependence on college fees were noted across the country. In 2023/2024, Ontario was the only province where the majority of college revenue (64.5 percent) came from fees, while all other provinces and territories relied more on provincial funding.
In 2023/2024, college fees accounted for the smallest share of total revenue in Nunavut (2.5 percent), the Northwest Territories (3.7 percent) and Quebec (7.5 percent).
Despite the large increase in total fees in 2023/2024, revenue from future fees could be impacted by federal and provincial policy changes. These policy changes include capping international student study permit applications and changing the eligibility criteria for the Post-Graduation Work Permit Program.
Colleges received their largest year-over-year increase in public funding in a decade in 2023/2024. However, public funding continues to decline as a share of total revenue.
Public funding – from federal, provincial, and municipal sources – increased by 2.1 percent to $8.5 billion in 2023/2024. Despite this rise, public funding’s share of total college revenue fell from 58.5 percent in 2020/2021 to 46 percent in 2023/2024.
In 2023/2024, colleges reported a second consecutive increase in investment income with all provinces and territories reporting positive returns on investment.
Total investment returns increased by nearly two-thirds (+65.8 percent) to $466.5 million in 2023/2024, following a record 110-percent increase the previous year.
The renewal of collective agreements, retroactive payments and the hiring of new staff to support increased student enrolment contributed to a record year-over-year rise in college salary and benefit expenses in 2023/2024.
These expenses increased by 9.4 percent to $10.5 billion in 2023/2024. However, they continue to represent a smaller share of total spending, falling from a high of 66.5 percent in 2020/2021 to 58.3 percent in 2023/2024. StatsCan
****************************************************************************************************************************
The National Association of Career Colleges (NACC) recently released the results of a survey on career college graduate work outcomes. The survey, conducted by Nanos Research, found that 80 percent of employed career college graduates are working in jobs directly related to their program of study and three in five graduates were employed within three months of graduation. About one-third of graduates were hired by the organization where they completed an internship or practicum. Despite being subject to more stringent regulation and greater oversight – something the sector overwhelmingly embraces – colleges are prevented from accessing the same supports as their public counterparts, NACC noted. “So, if the Prime Minister truly wants to provide ‘timely access to education and training,’ as he outlined in his mandate letters, it’s time to ensure that federal policies follow the facts.” This should start by ensuring career college learners have equitable access to federal student aid programs. Instead of limiting student choice, federal student aid policies should be aligned with these institutions that have a proven track record of delivering the workers Canada needs, NACC said. “Career colleges are eager to work with the federal government to create greater fairness and enable it to achieve its policy goals by delivering in-demand workers who will strengthen our economy for the long term.” NACC
The 11 leaders of the Université du Québec network and its member institutions have co-signed an article responding to Bill 1, the draft Québec Constitution Act. The authors call on the Government of Québec to remove Article 5 from the bill and to explicitly recognize academic freedom and autonomy within the constitution. In the letter, published in the Journal de Montréal, the authors explain that academic freedom and university autonomy is essential to fulfilling their institutional missions. They assert that Article 5 would jeopardize this by prohibiting universities from using their operating funds to challenge certain laws when needed to defend their mission. “This restriction would deprive them of their last resort: the ability to take legal action to defend their mission of teaching, research, and creative activity,” the signatories said. They point to incidents in the United States as examples of the risks posed by the bill as currently written. Journal de Montréal
Campus New Brunswick partnered with the national digital credential network MyCreds / Mes Certif, Canada’s national digital credential network. Through this initiative, funding from the New Brunswick Department of Post-Secondary Education, Training and Labour through CampusNB will support the onboarding of all CampusNB member institutions – starting with St. Thomas University – to MyCreds. This partnership will bring access to secure, portable digital academic records to postsecondary institutions across New Brunswick. Learners will have improved access to their academic records, empowering them in their academic and career transitions. The initiative builds on the successful precedent established in other provinces, where provincial support accelerated onboarding across all postsecondary institutions. By following this model, New Brunswick learners and graduates will benefit from consistent access to a modern, learner-centric digital credential platform that empowers mobility, supports academic and career transitions, and strengthens connections between learners, employers, and educational institutions. St. Thomas University
******************************************************************************************************************************
International students are an asset to Alberta universities
OPINION
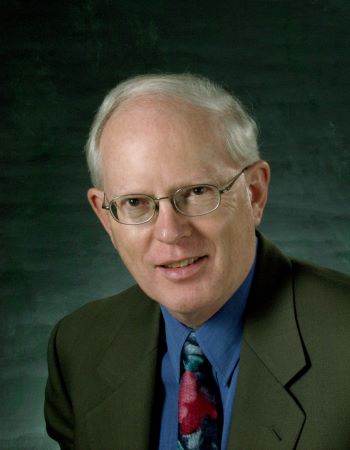
By Bill Flanagan
Bill Flanagan is University of Alberta president and vice-chancellor. This op-ed first appeared here in the Edmonton Journal.
International students have long been essential to the University of Alberta’s success. They enrich classroom discussion, strengthen our research enterprise, and contribute to the vibrant, global campus community that defines a top-100 research-intensive university. They also play a critical role in Alberta’s future workforce and economy.
Yet one misconception persists: that international students take away spaces from Albertans. This concern is understandable, but it is incorrect. In Alberta, the number of domestic students universities can admit is set entirely by the provincial operating grant. For example, the province funds just over 36,000 full-time domestic students at the University of Alberta.
Whether international enrolment rises, falls, or stays the same has no impact on how many domestic students we can admit. The two systems are completely separate.
In fact, international student tuition revenue strengthens our ability to educate Albertans: International undergraduates pay five times as much in tuition as domestic students, and their tuition more than covers the full cost of their education. Alberta taxpayers do not subsidize them.
This international tuition revenue directly supports the quality and breadth of programs available to all students. It allows us to hire professors, maintain specialized programs, expand course offerings, invest in modern laboratories, and support the student services all learners rely on. Without international students, we would not be able to sustain the world-class academic experience Albertans expect from their flagship university.
Alberta’s population has grown rapidly in recent years, and demand for university spaces has grown with it. That is why entrance averages in high-demand programs such as Engineering, Nursing, Science, and Business have reached historic highs. These pressures reflect population growth and the fact that provincial funding levels have not kept pace with this growth. It has nothing to do with international student enrolment.
Reducing international student numbers will not create additional spaces for Alberta students. The only way to create additional spots for Alberta students is through provincial funding that keeps up with Alberta’s rapidly growing population.
There are encouraging signs of potential new provincial funding to support growth in domestic enrolment. The government’s recent Expert Panel on Post-Secondary Institution Funding and Alberta’s Competitiveness recommended a modernized funding model that aligns provincial investment with student demand and the cost of delivering programs. If implemented, a model of this kind would fund enrolment growth and enable institutions to add seats, addressing Alberta’s urgent shortage of post-secondary spaces for its rapidly growing population.
The value of international students extends far beyond campus. They are among Alberta’s most important future citizens. More than 60 percent of international graduates from the University of Alberta choose to remain in the province after completing their degrees. They stay because they see opportunities here and want to build their lives and careers in Alberta.
These graduates are young, highly educated, and deeply engaged in key sectors of Alberta’s economy, including artificial intelligence, health sciences, energy, agriculture, engineering, and business. Many launch companies and create jobs. Others contribute to innovation and research that strengthen Alberta’s global competitiveness.
Their economic impact is substantial. Global Affairs Canada estimates that international students contribute nearly $2 billion annually to Alberta’s economy through tuition and local spending. They support Alberta businesses, enrich cultural life, and help make our province more connected and globally engaged.
In short, international students are an asset – not a constraint. They strengthen the University of Alberta, expand opportunities for domestic students, and contribute directly to Alberta’s workforce, economy, and communities. And at a time when Alberta is competing globally for skilled people, they represent one of our most promising sources of long-term talent.
Alberta’s universities succeed when they welcome the world, and so does Alberta. Attracting and supporting international talent is one of the strongest investments we can make in the province’s economic future, its workforce, and its global competitiveness. Edmonton Journal
******************************************************************************************************************************
If you start commercializing your research when it’s finished, you’re missing the point (By then, it’s already too late).
COMMENTARY
By Andrew Maxwell
Dr. Andrew Maxwell is the Bergeron Chair in Technology Entrepreneurship in the Lassonde School of Engineering at York University.
Most researchers still believe commercialization begins after the last experiment, after the patent filing, after the paper is finally accepted.
But if you wait until your research is “finished” to commercialize it, you are fundamentally missing the point – the point at which the research is still flexible, the technology is still malleable, and users can still shape what you build.
By the time most researchers start thinking about adoption, it is already too late to influence the decisions that drive commercial success.
All the critical decisions you lose when you commercialize too late
(And how each one would have changed the research or the technology.)
- You miss the decision about which feature should be optimized.
Impact on research: Early user input would have told you which technical pathway created real value. This could have redirected experiments, dropped unnecessary capabilities, or concentrated effort where it created adoption, not novelty.
- You miss the decision about the direction and magnitude of performance improvement.
Impact on research: Without user evidence, you don’t know whether to pursue radical performance gains or small reliability improvements. This leads to over-engineering (wasted years) or under-engineering (failing adoption thresholds).
- You miss the decision to align the technology architecture with real user needs.
Impact on research: Architecture, interfaces, workflow, integration points – all are determined early. Early conversations would have reshaped the prototype to fit the real world rather than an imagined one.
- You miss the decision to build in technical elements that increase motivation to adopt.
Impact on research: Adoption depends on behavioural drivers: visibility of outcomes, clarity of benefit, reduction of uncertainty. These need to be designed into the system. Late discovery makes this nearly impossible.
- You miss the decision to reduce perceived risks and switching anxiety.
Impact on research: You would have simplified installation, improved compatibility, reduced training, or built stronger reliability evidence into your experiments. These decisions shape the technology early; retrofitting them later is costly.
- You miss the decision to design the technology so it is actually easy to adopt.
This includes far more than integration. Early user input would have revealed multiple frictions:
- Integration into existing systems – leading you to modify interfaces, data formats, workflow timing, or hardware constraints.
- Ease of use – pushing you to simplify interactions, automate steps, or reduce cognitive load.
- Ease of maintenance – shaping design choices around robustness, repairability, downtime, and supportability.
- Training requirements – guiding you to embed instructions, simplify workflows, or reduce required expertise.
- Installation and deployment – prompting design for plug-and-play, modularity, or remote configuration.
Impact on research: Each of these insights would have changed your experimental design, engineering priorities, and prototype architecture. Once the research is complete, most of these adoption-critical features are extremely difficult – or impossible – to add.
- You miss the decision to embed observable, measurable outcomes that matter to decision-makers.
Impact on research: You would have captured the evidence that users, regulators, and partners actually need: return on investment, safety signals, compliance metrics, reliability thresholds. Once experiments are over, this data often cannot be recreated.
- You miss the decision to co-design the business model with the technology.
Impact on research: Knowing whether adoption depends on low upfront cost, trialability, shared risk, or subscription pricing would have changed your design targets and engineering choices.
- You miss the decision to modify the technology to fit the chosen business model.
Impact on research: A usage-based model may require telemetry; a pilot program may require modular deployment; a service-based model may require remote monitoring. These features must be designed early.
- You miss the decision about whether this technology should be licensed or spun out into a new venture.
Impact on research: Early evidence on integration needs, disruption potential, risk ownership, and stakeholder incentives would have guided the structural path. Choosing incorrectly – which happens often – leads to failure for reasons unrelated to scientific quality.
- You miss the decision to stop.
Sometimes the evidence shows there is no viable market for the technology.
Impact on research: Early clarity would let you pivot the research, focus on publishing, or redirect commercialization energy toward ideas that actually have adoption potential. Waiting until the end guarantees an expensive surprise.
A hard truth: even with the right process, most research will not be commercialized
Traditional academic commercialization succeeds only around four percent of the time.
A disciplined, adoption-centred process – the one we teach – can quadruple those odds.
But quadrupling four percent brings you to 16 percent, not 100 percent.
This is not a magic solution.
It is a method for:
- discovering failure earlier.
- avoiding wasted years.
- understanding adoption barriers before they are baked in.
- redirecting effort toward the projects with real potential.
The most common failure in research commercialization is timing.
People learn the truth only after nothing can be changed.
This process lets you learn the truth when everything can still be changed.
[Editor’s note: Andrew Maxwell teaches the Technology Commercialization Course as an open global classroom: to give researchers a practical, evidence-driven way to embed commercialization into research, not bolt it on after the fact. His course offers:
- how to identify your first user.
- how to shape technology for adoption.
- how to build business models that reduce risk.
- how to test assumptions before they become expensive.
- or how to know when not to commercialize]. Andrew Maxwell substack
*****************************************************************************************************************************
Micro-credential programs can help close skill gaps but only if created with employers and tailored for specific use cases
Micro-credentials can help close skill gaps and support equity but only if they are co-created with employers and tailored for specific use cases, according to an article by managers at the Northern Alberta Institute of Technology (NAIT).
In 2023, a cross-institutional team including NAIT, the Southern Alberta Institute of Technology and Bow Valley College conducted an Alberta-focused micro-credential research project funded by the Future Skills Centre to explore how employers and employees perceive micro-credentials.
The study drew on insights from over 500 survey responses and more than 50 interviews with stakeholders spanning manufacturing, trades, IT, finance, education, construction, emerging sectors and underrepresented communities.
The study showed that employers overwhelmingly still trust traditional credentials first, said the article by Partha Roy, Karla Barron and Scott Briggs at NAIT. Roy is market research manager, Barron is program manager of energy and environment, and Briggs is content generation lead.
Employers don’t use micro-credentials widely to make hiring decisions, assess employees or determine promotions, the authors said. “Instead, they see them as supplementary – useful when labour is tight or when traditional pathways are not meeting the moment.”
However sectors like tech or when a recognized degree is missing (for example, newcomers, career switchers or those re-entering the workforce), micro-credentials gain traction quickly, they noted.
Employers said they were more open to using micro-credentials to validate skills when faced with a talent crunch or when diversifying their hiring pipelines.
So micro-credentials are not replacing diplomas, “but they are increasingly filling the cracks in a fractured labor market,” the authors said.
Their research identified three key features of micro-credentials that matter most:
- Specific and focused in scope.
- Tied to authentic workplace assessments.
- Stackable or competency-based – ideally both.
“The idea is not just to teach but to verify, signal and connect to something bigger,” the authors said.
Unfortunately, what is happening on the ground is uneven, they pointed out. The digital icon? Mostly ignored. The metadata that could boost employer confidence? Largely unknown. “And while flexibility is valued, both learners and employers told us there is still a strong preference for in-person or hybrid delivery, especially for hands-on skills.”
Forget micro-credentials for the general population, the authors advised. Micro-credentials shine in specific use cases:
- Workers upskilling in response to tech or regulation changes.
- New immigrants or career changers needing to validate prior learning.
- People out of the labour market who need a fast re-entry point.
- Emerging roles where no established training yet exists .
Employers said that diversity and inclusion is one area where micro-credentials can be a powerful tool.
They are more likely to accept nontraditional credentials when trying to hire from underrepresented groups or where prior education may not align with Canadian standards. “That is a huge opportunity for both equity and economic recovery.”
However, many employers still do not understand what micro-credentials are or how they differ from regular certificates. They struggle to fit them into existing human resources systems. Collective agreements, professional bodies and regulators often do not know how to evaluate them or resist doing so.
This is not a technology problem but a systems problem, the authors noted. “Without cross-sector collaboration between industry, postsecondary institutions and governments, we risk building credentials that no one knows what to do with.”
Their research showed that, when demand for specific skills outpaces the supply of traditionally credentialed candidates, employers are more than willing to give micro-credential earners a shot.
This is especially true in emerging sectors such as artificial intelligence, cybersecurity or renewable energy, where traditional programs have not yet caught up.
It is also true for internationally educated professionals who need something tangible and Canadian to prove they are job ready.
And it holds for people who have been out of the workforce, whether due to caregiving, health issues or economic displacement, who are now looking to re-enter. For them, micro-credentials offer a way to rebuild confidence, signal current readiness and return with purpose.
In other words, micro-credentials are often most valuable when people are looking to pivot across sectors, across borders or back into the labour market, the authors said.
NAIT builds its clean energy micro-credential suite from direct conversations with employers in hydrogen, energy efficiency and retrofit sectors.
The resulting insights shaped short, targeted training aligned to specific job tasks, not just broad subject areas.
NAIT is embedding this training into larger pathways across trades, engineering and environmental careers. The result is employer-informed, data-backed and learner-focused programming. “It is not a cure-all, but it is a meaningful step toward building future-ready skills.”
The authors said their work on micro-credentials at NAIT revealed two important lessons:
- Microcredentials are helping us respond to skill gaps in real time. While traditional education programs are still adapting to the rapid changes in clean tech, these short, competency-based credentials give learners a way to build relevant skills quickly and step directly into roles where those skills are urgently needed.
- To be truly effective, micro-credentials must be built together with industry. When employers help define the specific skills and competencies they need, we can create training that’s not only relevant but also immediately valuable in the workplace.
For those working in continuing education, workforce development or training strategy, the authors said their research is saying:
- Start with insight. Do not build based on “vibes.” Use data, interview employers, scan job postings and validate with your own students.
- Design for specific use cases. Not all learners are the same. Micro-credentials are most powerful when they’re targeted and tailored.
- Co-create with employers. From defining competencies to vetting assessments, employers need to be partners, not just consumers.
- Make pathways visible. A single micro-credential is not a magic bullet, but when it stacks into something bigger, it becomes a bridge.
- Advocate for recognition. Collaborate with professional associations, labour unions and human resources professionals to ensure micro-credentials are integrated into existing recognition systems and not treated in isolation.
“The labour market is not just changing. It is fragmenting,” the authors said.
Roles are emerging faster than education systems can respond, and learners are piecing together careers from shorter experiences. Employers are desperate for people with the right skills but unsure where to look.
Micro-credentials will not solve all the challenges in this shifting paradigm, but if they are built with rigour, aligned with employer needs and treat them as part of a broader credential ecosystem, they can help make the uncertain a little more navigable, the authors said.
“Let’s stop asking whether micro-credentials are the future. They are already here; the question is whether we will use them wisely.” The evoLLLution
CANADA’S CURRENT & FUTURE WORKFORCE
Statistics Canada (StatsCan) released a report on new registrations, certifications, and pathway indicators of registered apprentices in Canada in 2024. The report indicates that new registrations have increased to 101,541 (+5.9 percent from 2023) in 2024, marking the fourth consecutive year of growth. The strong recovery, post the COVID-19 pandemic, in apprenticeship registrations highlights the sustained demand for skilled trades across the country, StatsCan said. Growth was noted in the provinces of Alberta, Ontario, and British Columbia and in the fields of electricians, plumbers, pipefitters and steamfitters, and automotive service workers. Declines were most prominently noted in Quebec and Nova Scotia. In 2024, new registrations increased year over year in 16 of the 24 major trade groups or remained relatively unchanged. Interior finishers (+27.9 percent), hairstylists and estheticians (+26.5 percent), construction workers (+24.2 percent), and early childhood educators and assistants (+16.7 percent) saw the highest growth. Conversely, machinists (-11.5 percent), stationary engineers and power plant operators (-9.1 percent), and landscape and horticulture technicians and specialists (-6.5 percent) saw the largest year-over-year declines. Levels in these groups also remained below those observed before the pandemic. Certifications of apprentices in 2024 stayed relatively steady with a slight increase to 46,971 (+one percent from 2023). Looking at the pathway indicators, the certification rate of apprentices increased by 1.1 percent, while the discontinuation rate declined by 0.3 percent. StatsCan
McMaster University’s DeGroote School of Business recently introduced a suite of new AI programs designed for professionals looking to integrate the technology into their careers. The programs are:
- The Master of Management in Applied AI and Data-Driven Decision-Makingis a part-time program designed to help managers lead data-driven initiatives, work effectively with analytics teams, and apply AI in real business contexts. This is not a technical program; no coding is required.
Tailored for professionals with at least four years of experience, the 20-month program blends in-person weekend sessions with online learning, giving students the flexibility to build new skills while continuing their full-time jobs. The first cohort begins in January 2026, and applications for future cohorts will be accepted on a rolling basis.
- A full-time program, Master of Management in AI and Analytics, is targeted at early-career professionals and recent grads.
The 16-month program provides hands-on training in tools such as Python, R, SQL, Tableau, and major cloud platforms. It’s designed to bridge technical data skills with business strategy, supported by real industry experience.
- The new Graduate Academic Certificate in Data Science, Applied AI and Organizational Leadershipis for working managers looking for a shorter, more focused introduction to these concepts.
Over four months, students take three courses and learn to design and implement actionable AI and data strategies using tools like Chatbots, AI Agenda, Azure AI, and Power BI. The program is tailored for mid-career managers looking to enhance their impact by leading AI adoption and driving organizational change. BetaKit
To help trades students better understand plumbing code, Fred Bretzke, an instructor at the Southern Alberta Institute of Technology (SAIT) transformed the 2020 National Plumbing Code appendix into a series of 3D-enhanced computer animation videos. Using computer equipment, digital tools and AI voice programs, he created 65 animations and eight holograms from the existing code appendix articles. The animations, which he uploaded to YouTube, are intended to serve as teaching tools for trades instructors. “Trades are very visually oriented,” Bretzke said. “Seeing things in 3D helps expedite learning and makes everything more accessible to the student.” Bretzke’s next immersive teaching project is “SAIT City,” a 3D set of commercial and residential buildings that could be used to teach multiple trades. SAIT
Six Nations Polytechnic (SNP) in Ontario announced the launch of an Integrated Employment Service at its new SNP Career Centre to support jobseekers, learners and community members. Delivered in partnership with Employment Ontario and Fedcap Canada, the service will offer coordinated wrap-around supports, such as employment counselling, training pathways, engagement with local employers, and individualized action planning. “The new SNP Career Centre and Integrated Employment Service will ensure that both Indigenous and non-Indigenous jobseekers have access to high-quality guidance, training options, and employer connections,” said Amy Gleiser, SNP Dean of Community, Health, Trades and Apprenticeship. Six Nations Polytechnic
Mount Royal University announced that StartWork – a collaborative initiative involving the university, the Government of Alberta, and Northpine Foundation – will be expanding thanks to new funds from its partners. Under the program, 40 refugees voluntarily have transitioned from Income Support to StartWork, accessing tailored support and distinct employment paths through expert community partners. This has enabled them to gain vital Canadian work experience and begin building sustainable livelihoods. The expansion will create space for up to 300 people, with plans to support a similar number of people in future contracts. The program offers refugees four career paths (hospitality and food services, residential and commercial cleaning including commercial kitchen fire inspection, warehouse readiness and forklift certification, or carpentry) that they can pursue, each of which enables them to gain the certifications, skills and confidence they need to transition into jobs. The program also offers access to courses that develop life skills in areas such as driving, language and networking. Mount Royal University
The Charlottetown, P.E.I.-based Canadian Alliance for Life Sciences Training and Skills Development (CASTL) recently announced the creation of the CASTL National Training Advisory Committee (NTAC), an independent group of experts convened to provide strategic advice on the direction of CASTL's national training initiatives. Comprising 13 members, the NTAC is designed to represent a range of expertise, including leaders in advanced biofabrication, biologics, workforce development, education, and innovation. Members will serve two-year terms, renewable. The NTAC will advise CASTL on the strategic direction of its training activities and provide insights into emerging skills needs within the biofabrication and biotechnology sectors. The NTAC will also offer perspectives on CASTL's specialized training initiatives and the future of the biofabrication talent pool in Canada. CASTL
The Institute for Research on Science, Society and Public Policy (ISSP) at the University of Ottawa recently launched the Learning Hub, a resource developed and managed by ISSP to help emerging and established leaders acquire the knowledge and skills needed at the science, society and policy (SSP) interface to address major decision-making challenges. Whether you are a beginner or want to deepen your knowledge of advanced SSP topics, this self-study resource will be helpful. The training hub includes training modules linked to the intersectoral activities conducted by the ISSP. These resources include video recordings of conferences and events, as well as open-access scientific and policy publications. The resources have been organized into self-directed modules to best meet user needs, including an introductory module to present key SSP concepts (including the history and current state of SSP in Canada) for beginners (available now), and more advanced modules organized around specific SSP-related themes (coming soon is SSP for researchers, research administrators, policy advisors, diplomats and other leaders at the interface of SSP (fees may apply). Learners wishing to receive an ISSP certificate of completion must complete all components of a module and then participate in an in-person ISSP-facilitated discussion group. Further details can be found on each module page. ISSP
******************************************************************************************************************************
Canadian workers express a mix of concerns, skepticism and cautious optimism about AI-powered automation displacing workers
Canadian workers have a mix of concern, skepticism and cautious optimism about automation by artificial intelligence displacing workers, according to a national survey from the Ottawa-based Future of Good media and research organization.
The organization fielded a survey, with the Angus Reid Forum, designed to assess public attitudes and perceptions about the AI-related threat of job displacement.
Scott Schieman, professor of sociology and Canada Research Chair at the University of Toronto (U of T), and Alexander Wilson, PhD student in sociology at the U of T, wrote about the survey in an article in The Conversation.
The survey asked respondents:
“A CEO of a major AI company recently made this statement: ‘AI could wipe out half of all entry-level white-collar jobs and spike unemployment to 10 to 20 per cent in the next one to five years.’ How likely do you think this is?”
The quote came from Dario Amodei, CEO of Anthropic, who was interviewed in an Axios article in May. The central thrust of the article was the imminent AI-related turbulence in the world of work.
In the survey, Canadian workers expressed mixed reactions to that dismal scenario: 16 percent felt it was “very likely,” while another 48 percent said it was only “somewhat likely.” The remaining 36 per cent said it was “not too likely” or “not at all likely.”
The survey then asked open-ended follow-up questions to gather qualitative insights about the ways that people are thinking and feeling about the AI threat. Most respondents expressed a pessimistic outlook, but a significant minority contrasted their view with optimism.
A common thread among pessimistic responses was concern over corporate greed and profit.
“Companies are always looking to reduce cost and improve efficacies, so there is a strong probability this is going to happen in many organizations over the next five to 10 years as AI continues to be used,” said a 66-year-old clinical manager.
Others were concerned about the looming loss of dignity and respect for workers. “Executives do not see the value of the human mind compared to a machine,” a 53-year-old senior government policy analyst said. “It shows they have no concern for employees, just profits.”
Not everyone was so gloomy. Many expressed optimism about AI and the human capacity to adapt and evolve.
“AI is not a replacement for humans,” said a 54-year-old community television producer, while emphasizing that rather than replace humans, AI “should allow humans to accomplish more at their jobs.”
Others shared this confidence, drawing parallels to other historical changes in technology. “The job market will adapt as needed,” speculated a 34-year-old service officer, “switching to different roles that match the current technology, just as we have done in the past.”
“These findings show that, despite sensational headlines about AI and job loss, Canadian workers’ perceptions about the issue are complex,” Schieman and Wilson said.
“It’s clear that the emotional landscape of work is filled with frustrations about corporate priorities and skepticism about whether workers will be protected. And yet, our survey found traces of resilience in the belief in the essential humanness of work.”
Philip Cross, senior fellow at the Macdonald Laurier Institute, in a 2023 report pointed out that machine automation has been feared for its impact on human jobs since the Industrial Revolution began. Earlier eras of automation disrupted employment patterns in farming and factories, but overall job growth actually accelerated as higher incomes drove the expansion of other industries, he noted.
“Despite that experience, there are numerous forecasts that the deployment of AI will lead to widespread job losses,” Cross said.
Compounding the anxiety of potential job losses is the fear that AI will displace middle-class jobs and that the rewards from the widespread deployment of AI will accrue to a small number of people who own the capital and will thereby increase inequality.
There is a long history of erroneous predictions about new technologies leading to massive job losses for workers, Cross said.
While every recession in the past century has been at least partly blamed on automation, these pessimistic forecasts were all incorrect because of what economists call “the Luddite fallacy,” which ignores the fact that productivity gains from technological innovation always have immediately or eventually generated more income and jobs, he said.
Over the last two centuries job losses on farms and factories that resulted from new technologies were balanced by workers upgrading their skills and moving to new occupations where demand was rising due to higher incomes generated by productivity gains.
Few of the lost jobs were missed as most of the work replaced during the early Industrial Revolution was repetitive, routine, and often dangerous, Cross said.
“While economists and pundits worried for decades that robots and automation would destroy millions of jobs, outside of cyclical recessions employment rates have risen steadily, to record highs.”
Much of the difficulty of forecasting the impact of technology on the labour market stems from the challenge of predicting how technology itself will evolve, Cross said.
Overall, AI is likely to make workers more productive and therefore more desirable to employers. Furthermore, the implementation of AI technology is likely to roll out slowly, which will help employers and workers adapt to its use, he said.
Past history shows even the most transformative technologies, such as electricity or the internal combustion engine, require decades to be widely diffused. A prolonged period of adaptation seems to be inevitable for AI, Cross said.
While the potential capabilities of AI are often exaggerated, human abilities are routinely underrated, he said. Humans retain key abilities that machines cannot duplicate or replace. Even in highly technical fields such as machine learning, artificial intelligence, and cloud computing, human beings are underrated.
“Machines may replace some jobs, but humans are too intelligent, creative, versatile, and adaptable to not find interesting work to do,” Cross said. Future of Good, MacDonald Laurier Institute
SECTOR SIGNALS: The health care sector
Report offers a blueprint for creating a resilient, sustainable health care system for Canada
Canada’s public health care system is under severe strain and the country needs a resilient, sustainable system that’s adaptable to existing and future pressures, according a report by Deloitte.
Despite record increases in health care spending across all provinces, rising demand for services and public expectations are outpacing the system’s ability to deliver, said the report, The resilient health system: A blueprint for sustainable healthcare delivery, released last year.
Public opinion and international rankings continue to indicate that Canada falls short on outcomes and cost-effectiveness.
While Canada’s peers across the globe are largely experiencing the same pressures, in many cases bold steps are being taken to make the health and care system more resilient.
Canada already commits approximately 40 percent of all government spending on health, and this expenditure is only projected to increase, putting provincial governments and other critical social programs under strain, the report said.
“The critical issue is not necessarily how much is spent but rather how resources are allocated and used to drive outcomes,” according to the report.
Continuing to apply ongoing growth and funding, while also expecting operational efficiencies and cost reduction solutions, is clearly untenable on their own, the report said. “Without fundamental changes to how our health care system operates, we risk reacting to urgent system failures and pouring ever more resources into the system for diminishing returns.”
A truly resilient health system prioritizes health outcomes, reshapes response to challenges – both from the supply and demand perspective – and directs spending to value, the report said.
According to the report, achieving a resilient healthcare system needs a structured approach that better aligns fiscal, operational and clinical efforts. It also requires balancing stakeholder interests and addressing well-known and deep-rooted issues such as funding flows, physician compensation and system structure.
Currently, there is limited focus on driving sustainability, flexibility and financial improvement and subsequent full return on investment, the report noted. “The system’s well-known fragmented and, very often, siloed structures hinder collaboration and integration, while limited competition, and lack of incentives, stifles innovation.”
The system has developed a growing dependency on funding increases, often at the expense of pursuing system transformation or turnaround, the report said.
For example, Canada has one of the highest rates of lower limb amputations in similarly funded and organized health systems, the report points out.
While evidence suggests that early intervention and better management of diabetes and diabetes-related conditions could fundamentally change the outcomes for these patients, Canada’s system prioritizes paying for amputation as opposed to the care required to keep these patients and their caregivers happy, healthy and as productive members of society and the economy.
“Unfortunately, there are numerous examples such as these where the health systems pay for discrete and siloed services, resulting in more expensive and poorer patient and society outcomes.”
In short, Canada’s system is structurally siloed, prioritizing treatment and more urgent care over lower-acuity models such as home-based care and prevention, the report said.
Developing a resilient healthcare system requires shifting away from hyper-localized, tactical, and opportunistic solution and toward systemic, strategic and intentional approaches, according to the report.
This includes focusing on outcomes rather than inputs, planning for the future through strategic investments in infrastructure, and building cross-sectoral collaboration to align services and resources effectively.
A resilient system operates a more distributed health network model – aligning and connecting hospitals, primary care and community health partners to deliver holistic, sustainable solutions that meet patient needs while ensuring the operating model is the right size and shape for patient and population needs.
According to the report, these main components are required to achieve a resilient health care system:
- Flexible, multi-year fiscal planning cycles and resource flows focused on outcomes.
Outdated funding and data rules remain significant barriers. Current structures often limit the transfer of money between providers, limiting the ability to reallocate resources towards preventative measures, even when doing so saves costs and improves care.
- Implementing a performance and management framework.
By focusing on a defined set of measurable outcomes, this framework ties multi-year funding to clear success indicators, enabling health care leaders to align investments with meaningful objects.
Key benefits of a resilient healthcare system for policymakers and funders include:
- A clear link between spending and value.
Instead of focusing solely on activity, a resilient system connects spending to meaningful outcomes, such as improved access, quality of care, broader coverage, and adoption of new evidence-based treatments.
- Rebuilding trust or sustainability and cost control, by restoring trust between funders and providers through accountability and transparency.
- Improved quality of care and outcomes.
Integration across providers creates a more coordinated and patient-centered approach to care, bridging gaps between services and regions and addressing disparities in access and outcomes.
Benefits of a resilient healthcare system for provincial health care leadership include:
- Clear definitions of success and accountability.
Linking health care spending to measurable outcomes over multi-year funding cycles ensures accountability, addresses the frustrations around undefined expectations, and helps track the effectiveness of investments.
- System-wide collaboration and resource optimization.
Structured channels for sharing best practices, data and innovations across provinces enhance cross-system collaboration. This reduces redundancies and enables strategic resource allocation that focuses on prevention, coordination, co-investment and care optimization.
- Sustainable investments with financial predictability.
Flexible funding models allow leaders to address root causes through sustainable initiatives and not worry about whose budget or what unintended consequences might occur when caring for a patient in the optimal sector of the health system that matches their unique needs.
Benefits of a resilient health care system for care delivery providers include:
- Accountability through outcome-based metrics.
These metrics help align organizational goals, track progress, and support informed decision-making by boards and leadership.
- Flexibility to innovate and adopt.
Operational and funding flexibility enables providers to explore new approaches and implement new initiatives.
- Collaboration to access innovation and resources.
Cross-provider collaboration breaks down silos to allow providers to share resources and adopt best practices.
The report provides several examples of internal levers that health care institutions should be currently considering to maintain financial sustainability, and external levers to address challenges affecting health care’s long-term sustainability.
“The health systems of the future require a laser focus on what creates patent value and what does not,” the report said.
Change will require leadership, clarity of purpose, determination, and the acceptance of calculated risks by senior leadership teams prepped with the right data and processes to effect change, according to the report..
Change also requires clarity from governments on policy and a focus on understanding the outcomes they ae are trying to drive with more emphasis on measurement and accountability and less focus on process.
Concluded the report: “A resilient health system is not only the right thing to build but necessary to care for today and tomorrow’s patients.” Deloitte
******************************************************************************************************************************
Canada’s first Indigenous-led faculty of health sciences is taking shape on James Bay coast in northern Ontario
Queen’s University, the Weeneebayko Area Health Authority and the Mastercard Foundation are building what will be Canada’s first Indigenous-led faculty of health sciences campus in Moosonee, Ont.
The goal is to recruit, train and retain health professionals in-place, for the communities they serve – across nursing, medicine, midwifery, rehabilitation and paramedicine.
“This is not simply about filling jobs; it is about reshaping systems so care is delivered by people who understand the land, language and culture of those they serve,” Jamaica Cross, a Mohawk physician educator from Tyendinaga who leads Queen’s–Weeneebayko Health Education Program (Q-WHEP), wrote in an article in Policy Options.
In the James Bay and Hudson Bay region, too often, care is delivered by rotating agency nurses and locum physicians on short contracts, who fly in and out, she said.
The infrastructure to provide care exists – a new hospital campus is under construction – but the workforce to sustain it does not. “Patients are frequently evacuated hundreds of kilometres south for basic services that could, and should, be provided closer to home.”
Q-WHEP’s program is co-designed with the local health authority, Indigenous leadership and community knowledge-holders so that graduates can fill projected vacancies – not just in hospitals, but across community and primary-care systems.
However, barriers remain, Cross noted. Health and education remain in separate ministries, with different budgets, timelines and metrics. Funding for student seats and funding for practice positions seldom align.
Philanthropic investment (including a $31-million contribution from the Mastercard Foundation) has enabled early development – but sustainable public-infrastructure funding remains uncertain.
In many northern and Indigenous communities, there is no comprehensive data on regional providers, turnover or part-time versus full-time practice. Workforce projections are too often built on patchwork sources.
Cross said these challenges are solvable – “ if we design governance, data systems and funding structures that work together.” To get there, she said that governments, health authorities and educational institutions should work together to do the following:
- Integrate Indigenous community data into national workforce datasets so that planners can identify and reduce service gaps.
- Treat rural and Indigenous training pathways as core workforce strategy, not just equity initiatives. Evidence shows health professionals trained in rural or Indigenous settings are significantly more likely to practise long-term in those settings.
- Align funding across ministries so that seat creation, clinical-placement funding, job creation and wraparound student supports are planned together – to set communities up for success.
- Leverage interprofessional education – training nurses, physicians, midwives, paramedics and therapists together – to reduce duplication and increase system adaptability.
“What we are building on the western James Bay coast is a local solution and a national prototype,” Cross said. “It shows Indigenous-led, data-informed, community-driven workforce planning is possible – but only if education systems, health systems and policy frameworks move in tandem.”
By 2045, Cross said she envisions a Canada where shared governance tables replace silos; where education institutions, health authorities and Indigenous governments co-design workforce strategies; and where predictive, interoperable data systems – rooted in principles of data sovereignty – anticipate workforce gaps before they become crises.
Training infrastructure will be distributed and embedded in communities, not confined to urban centres, she said. Micro-campuses like Q-WHEP will be standard, not exceptional. Career pathways will be fluid: from early exposure in high school, through college or university, to clinical practice and leadership.
Indigenous and community-based knowledge will matter in credentialing, Cross said. Every partnership between government, post-secondary institutions and communities will include shared-outcomes mechanisms, transparent reporting and sustained dialogue.
“In this future, health systems will breathe – they will be adaptive, community-informed and predictive, not reactive,” she said. Communities will be fully staffed with local professionals delivering culturally safe, trusted care.
Health equity indicators – infant mortality, chronic disease, mental-health outcomes – will improve measurably. Indigenous leadership in education and care will be normalized, not exceptional.
“We’ll know we’ve arrived when we no longer talk about reconciliation as a goal – because it is simply how our systems work,” Cross said.
“Because, in the end, alignment isn’t about numbers – it’s about relationships. Education and workforce planning come full circle when all learners see themselves in the system they serve, and every community sees its reflection in the care it receives.” Policy Options
******************************************************************************************************************************
Virtual healthcare provides benefits for Canada’s healthcare system but fragmented governance landscape needs addressing
Virtual healthcare has rapidly expanded across Canada, improving convenience and access for many but also creating a fragmented governance landscape, according to report by the C. D. Howe Institute.
Provinces differ widely in how they regulate, fund and integrate virtual care, making cross-border delivery complex and leaving major gaps in continuity of care for patients navigating their journey through the health system, the report said.
The report’s authors are Katherine Fierlbeck, fellow-in-residence, at the C. D. Howe Institute, and Rosalie Wynoch, associate director of research.
Despite efforts to align public systems with modern care delivery, large loopholes in how “insured services” are defined by provinces in practice have enabled significant growth of private, for-profit virtual care, they said.
These services operate both within and across provinces, raising concerns about equity, data fragmentation and uneven access based on patient resources or employer benefits.
As virtual care becomes a permanent feature of the healthcare system, provinces must strengthen regulatory frameworks, protect continuity of care from fragmentation, and clarify the scope of insured services.
“Choices made now will determine whether virtual care reduces access gaps and enhances integration or contributes to greater inequity and system fragmentation,” Fierlbeck and Wynoich said.
“Virtual care” is generally defined as any interaction between patients and/or members of their circle of care, occurring remotely, using synchronous or asynchronous forms of communication.
While virtual care and “telemedicine” were not entirely unknown before COVID-19, formal and informal decisions to limit social interaction during the pandemic drove both patients and providers to engage with various modalities of virtual care on a much wider scale, the authors said.
As the pandemic abated, patient and provider satisfaction with this mode of care led to ongoing adoption and scaling-up of some of the temporary and experimental approaches that emerged in 2020.
“Virtual care offers the opportunity for provincial and territorial jurisdictions to bolster primary care access where it is stretched thin, but it also threatens to undermine their ability to shape healthcare in a coordinated and comprehensive manner,” the authors said.
British Columbia and Newfoundland and Labrador have the highest uptake of virtual care, followed by Nova Scotia, New Brunswick and Ontario, according to the report. Quebec and Prince Edward Island have the lowest usage, with more than 70 percent of people only accessing in-person appointments.
Virtual care “is a substantive challenge to the way healthcare systems as a whole are structured. Virtual care has opened more loopholes in the single-tier system of healthcare grounded in the Canada Health Act,” Fierlbeck and Wynoich said.
Specifically, the way in which virtual care works across geographic space (provincial boundaries), time (asynchronous and episodic care), and payment mechanisms (such as employer-based plans) has facilitated the growth of private for-profit, direct-to-patient care.
In contrast to in-person care within single jurisdictions, where physicians had to declare whether they wished to work within or outside of the public insurance system at any given time (except Ontario, which does not allow this option), the ease of cross-jurisdictional care provision means that physicians can work both in and out of “the public system.”
In effect, they may work within the public system in one provincial or territorial jurisdiction, and outside of it in another.
The reason that this is now problematic is that, if it is convenient and financially advantageous to provide simple and uncomplicated services virtually in another province, physicians and nurse practitioners may choose to limit their working hours in the public system, thereby reducing provider resources in the public system across the board, Fierlbeck and Wynoich noted.
At the same time, virtual care increases the mobility of the limited provider workforce and could facilitate better access in rural locations and after-hours across time zones.
Since virtual care does not require full-time hours, it has the potential to increase retention of the health provider labour force both young and old, by allowing the flexibility to reduce total workload or care for young children.
“Virtual care is rapidly changing the landscape of healthcare in Canada,” the authors said.
The advantages of virtual care are considerable, but the question remains: who will benefit the most from it?
The expansion of virtual care means that governments will have to continue to think about fine-tuning their respective regulatory frameworks to ensure that virtual care pathways work as seamlessly as possible, Fierlbeck and Wynoich said.
Provinces would be well-advised to better articulate precisely what it is they wish to achieve with the potential that virtual care promises, they said. Better access for unattached patients? More convenient access for discrete cohorts? A more longitudinally integrated system of care? Better equity? Or perhaps economic productivity gains independent of health outcomes?
“In Canada, the key question is how federal and provincial/territorial legislation and regulatory requirements affect the provision of virtual care across provincial boundaries, and the consequences of these new pathways of delivery,” the authors said.
The current landscape of virtual care in Canada is characterized by significant provincial/territorial variation and considerable regulatory complexity, Fierlbeck and Wynoich said.
Provincial and territorial jurisdictions have taken different approaches to contracting with commercial providers, defining insured services, setting billing codes, and regulating cross-border provision.
“The sheer volume of laws, regulations, professional standards and licensing requirements – and the inconsistencies arising from their interaction – means that coordination between provincial/territorial jurisdictions and ongoing adaptation of policy will be required as virtual care evolves,” the authors said.
Many of the concerns related to continuity of care, rapid access to treatment, and integrated patient records affect both public and private channels. Virtual care both complicates and facilitates these goals: virtual delivery goes hand-in-hand with digital patient records and enables multi-provider coordination and asynchronous communication.
However, the potential for both public and private providers to treat a patient, along with the potential for data fragmentation if records are not shared across channels, complicates integration and continuity and raises privacy concerns about other potential uses of patient medical information.
Policy should encourage complete integration of information across providers while limiting the use of individual or identifiable patient data to appropriate and relevant uses, Fierlbeck and Wynoich said.
Further, guidelines for the provision of virtual care should require the ability to refer to in-person primary care, with clear pathways for continuity of care (particularly for provinces that do not currently have a robust continuity of care requirement as part of virtual care practice standards).
Provinces should approach virtual care as a useful tool to fill gaps in care and improve access, though there are potential trade-offs that should be monitored and managed where necessary, they said. These trade-offs include access and equity, public/private provider labour market dynamics, and public healthcare delivery balanced with public fiscal sustainability.
“Regardless of who pays, virtual care has significant potential to reduce inappropriate hospital visits and fill gaps in access to primary care,” the authors said.
About 17 percent of Canadian adults do not have a regular healthcare provider and more than three-quarters cannot access same- or next-day appointments and find it difficult to access care outside regular business hours.
One in seven emergency department visits could be managed in primary care settings, and over half of those could potentially be managed virtually.
Fierlbeck and Wynoich said their analysis clearly shows that virtual care has net benefits for Canadians – “it is a valuable addition to the healthcare system that can improve access, convenience and efficiency when appropriately integrated and governed.”
“The challenge for policymakers is not to resist the growth of virtual care or to choose definitively between public and private models, but rather to ensure that virtual care, in whatever mix of public and private provision emerges, serves the goal of affordable and equitable access to quality healthcare for all Canadians.”
What is required is ongoing policy innovation, interprovincial cooperation, systematic evaluation, and a willingness to adapt regulatory frameworks as evidence and experience accumulate, Fierlbeck and Wynoich said.
“Virtual care is neither a panacea that will solve all access problems nor a threat that will inevitably undermine the medicare system. It is a tool – and like any tool, its ultimate value depends on how skillfully and thoughtfully it is used.” C.D. Howe Institute
****************************************************************************************************************************
Canada must address significant gaps in health workforce that will worsen over the next 10 years without action
Canada has a significant gap in its health workforce that, if no action is taken, will worsen over the next 10 years, according to a government-led study.
The Canadian Health Workforce Education, Training and Distribution Study – the first pan-Canadian study of its kind – highlights the even larger gaps in rural and remote communities, the limited training capacity in the North, and the unique challenges of building the Indigenous workforce.
The study’s terms of reference were approved by the Conference of Deputy Ministers in January 2024.
Study oversight was carried out by the federal-provincial-territorial (FTP) Committee on Health Workforce and an FPT Project Team consisting of four provincial and territorial (representatives, the Canadian Institute for Health Information, Health Workforce Canada, and Health Canada, and was chaired by Dr. Geneviève Moineau, Chief Medical Workforce Advisor.
An important interdependence exists between provincial and territorial jurisdictions and Indigenous partners such that addressing health workforce challenges can only occur with collaboration across the country, the study said. “Health professional education and training capacity must increase now.”
Moving forward, Canada must establish:
- the ability to plan with a strong foundation of data on health professionals in training and in the workforce.
- integrated health workforce modelling.
- a health professions education and workforce planning collaborative council including representation from ministries of health and education and Indigenous partners.
- engagement with educators, regulators, accreditors, employers, certification bodies and health professions associations to enable the changes required to address the health care needs of the populations of Canada.
The scope of the study includes five professions engaged in primary care for which health workforce information was available from the Canadian Institute for Health Information, including nursing (licensed practical nurses, registered psychiatric nurses, registered nurses and nurse practitioners), occupational therapy, physiotherapy, pharmacy and physicians (with a specific focus on family medicine).
First Nations, Inuit and Métis Peoples experience significant disparities and challenges in accessing health professions education and training opportunities in Canada, according to the study.
Obtaining the education and training data for the five professions engaged in primary health care from most sources was very difficult, the study noted. There were significant variations in the data collected from various sources and they also differed significantly by profession, even in the same jurisdiction.
There was significant missing data on the four nursing categories. “The inability to confirm program capacity information for nursing, Canada’s largest group of regulated health professionals, is of significant concern. Program capacity is essential information to support health workforce education planning,” the study said.
The size of first year enrolment and graduation cohorts in the health professions examined is generally increasing at a slow pace, if at all, between 2018-19 and 2022-23, according to the study.
The number of graduates in physiotherapy, occupational therapy, pharmacy, licensed practical nurses (LPN), and registered psychiatric nurses (RPN) programs had zero to two-percent increase per year while family physicians had a 2.5 percent increase, and registered nurse (RN) programs had a five-percent increase.
The only significant increase noted was for nurse practitioners (NP) who had a 13-percent annual increase over four years.
Based on available data, the average annual growth in the projected workforce supply from 2022 to 2034 ranges from 1.1 percent for pharmacists, 1.3 percent for RNs, 1.7 percent for occupational therapists, 1.8 percent for family physicians, 1.9 percent for LPNs, two percent for RPNs, 2.1 percent for physiotherapists, and 4.1 percent for NPs.
The study found there is a current need for almost 23,000 more family physicians (49 percent increase from current supply), 14,000 more licensed practical nurses (12-percent increase), 2,700 more nurse practitioners (35-percent increase), 28,000 more registered nurses (10-percent increase), 500 more registered psychiatric nurses (eight-percent increase), 2,000 more occupational therapists (12-percent increase), 2,600 more physiotherapists (10-percent increase), and 1,700 more pharmacists (five-percent increase).
Nurse practitioners and physiotherapists are the only in-scope professions who are projected to have additional capacity by the end of the projection period.
Additional scenario analyses, exploring the potential future circumstances that may impact projected workforce supply-demand gaps, show that increasing population size and disease prevalence would substantially increase the projected gaps across all professions.
Further, expanding the potential for nurse practitioners to increase primary care attachment could also increase demand and the gap for that profession, while reducing demand and the gap for family physicians.
Lastly, early retirement in the professions would significantly reduce supply, thus widening the workforce supply-demand gaps over time.
“Across most occupations, the current state and projection results show substantial supply-demand gaps now and over the next 10 years,” the study noted.
Proportionally, the needs of rural and remote communities are higher, the supply is lower, and the gaps will increase over time.
The shortage of physicians in Canada is not surprising as Canada has been underproducing medical graduates for decades, the study said.
According to the 2023 Organisation for Economic Development and Co-operation (OECD) Health Report, Canada has 2.8 practising physicians per 1,000 population with the OECD average at 3.7 per 1,000 population. Norway has 5.4 per 1,000 population.
“Family physicians are key to the provision of primary care in Canada,” the study said. Yet In 2024, the C. D. Howe Institute reported that Canada currently has a deficit of 13,845 family physicians.
Nursing is the largest group of regulated health professionals in Canada, the study said. “Since the nursing profession is fundamental to a functioning health care system, educating a strong nursing workforce must be a priority. All four nursing categories need to increase their education seats to meet current and future population needs.”
Nursing education programs face challenges finding faculty and clinical resources including preceptors and placements, and health care settings are strained to accommodate students, resulting in attrition from nursing education programs and a failure to retain nurses once they are licensed and registered to practise.
Many challenges and barriers exist in the provision of education for all in-scope health professions and include, but are not limited to:
- the need for an increased number of training seats in an environment with a limited number of teachers, faculty members and preceptors.
- a scarcity of clinical placements.
- lack of investment in simulated learning opportunities.
- difficulty accessing the required number of patients.
- lack of remuneration or incentives for preceptors.
- insufficient administrative resources and funding.
Opportunities for innovation in health professions education include:
- targeted admission support for students who are currently underrepresented.
- on-line, virtual or distance education to accommodate students who are from various geographic locations.
- programs or rotations offered in rural and remote areas supervised by local health professionals.
Curricular design flexibility is apparent with accelerated pathways, bridging and “learn as you earn” programs as well as direct entry primary care medical education programs.
Education in interprofessional and First Nation, Inuit and Métis community settings are critical innovations for more integrated team-based care.
Integrated and collaborative policies across education and health service delivery can coordinate optimal health workforce outcomes, the study said. This interprofessional form of planning is in contrast to the usual siloed health profession-specific approaches.
Many countries are moving in this direction. The United Kingdom, Brazil, Australia, and Norway have legislated mergers between previously siloed sectors, such as education, accreditation, health and social service delivery systems and government.
The study’s request for information on the education and training capacity has reinforced the need for a standardized approach to data collection for health professions education across Canada.
“Except for physicians, is not possible to follow a health professional from training through practice and retirement.” This is a significant limitation in health workforce planning as jurisdictions are unable to track graduates into and out of the workforce, or movement between categories of professionals (such as, LPN to RN or RN to NP) or between different professions altogether (such as, physiotherapists or occupational therapists to medicine).
As jurisdictions have separate ministries of education and health, collaborative data sharing and health workforce planning are not inherently part of the departmental structures.
“This must be addressed for health professions education and training to respond to the health care needs within the jurisdiction.”
The study made several recommendations, including:
- Education, training and health workforce data.
A minimum data standard on health professions students and their education programs should be created and required for all health profession programs to complete and report on.
Data on health professions students and their education programs should be available to those who undertake health workforce planning.
- Health professions education and training planning.
Significant increases in education and training seats are required to meet the current and future demand for nurses, occupational therapists, physiotherapists, pharmacists and family physicians in Canada. Specific gaps and needs must be determined by provincial and territorial health profession education and health workforce planners.
- Health workforce projection modelling.
A federal-provincial-territorial community of practice for health workforce modellers in Canada should be developed to enable the application of new technical approaches to modelling and the use of different data and assumptions that would generally improve health workforce planning at various levels.
Integrated supply and demand projection models for interprofessional primary care teams should be created based on population health needs to improve decision makers’ ability to develop interdisciplinary care teams that optimize the health workforce.
- Rural and remote education.
The minimum data standard on health profession students should include information regarding student location at the time of application, during education and practice location.
A rural and remote health professional education and training network across provinces and territories should be established to enable collective sharing of innovative practices and solutions.
Sustainable resourcing mechanisms that support the long-term implementation of Indigenous-led recruitment and retention strategies for roles based within Indigenous communities and nations, that contribute to health workforce education and training, must be established.
- Employer role.
Health care employers should be ensuring the successful transition of new graduates and provide support and mentoring as they enter into practice.
- Health professions role.
Accreditation and regulation of health professions education must adapt as quickly as necessary to align changes to the education and training of health professionals to respond to societal needs.
Health professions education leaders need to work collaboratively to accelerate interprofessional educational transformation aligned with primary care competencies. Creating a new structure to break down the silos that currently exist would be beneficial.
- Ongoing study.
Ongoing work to access and create health professions education and training capacity data for cyclical reporting should be undertaken to help inform health workforce projections at a pan-Canadian level.
“Canada clearly has urgent work to do to address the current and future gaps in the number of health professionals studied,” the study said.
A commitment to establishing robust data requirements, and collaboration between health profession education and workforce leaders, are key to supporting the complex adaptive system required to succeed in providing the health workforce Canada needs.
“We have a strong workforce; we must now find a way to better leverage those strengths and innovate at the same time.”
An ideal future state for health professions education and workforce planning is one where a minimal data standard exists that allows knowledge of the individual as a trainee and a worker along their career trajectory.
Data would be regularly inputted from appropriate sources to allow cyclical adjustments to databases to help adapt projections and implement any required changes in education seats and other parameters.
Second, an interprofessional health profession education and workforce planning collaborative council is established including ministries of health and education, Indigenous leaders, employers, regulators, accreditors, educators, learners and communities to collectively address the health and health care needs of Canadian populations.
Third, a transformative learning health workforce education system is created where timely adaptations of policy decisions are based on a regular stream of robust data to inform and enable adjustment of assumptions for best modelling and predictions is possible.
“With collaboration and coordination amongst all key stakeholders, Canada can reach the goal of caring for Canadians by educating Canada’s future health workforce.” Govt. of Canada
R$
Events For Leaders in
Science, Tech, Innovation, and Policy
Discuss and learn from those in the know at our virtual and in-person events.
See Upcoming Events
You have 0 free articles remaining.
Don't miss out - start your free trial today.
Start your FREE trial Already a member? Log in
By using this website, you agree to our use of cookies. We use cookies to provide you with a great experience and to help our website run effectively in accordance with our Privacy Policy and Terms of Service.